Cushing syndrome occurs when a body acquires high levels of cortisol levels for a long time. Hence, it is also known as hypercortisolism. This is not one disease, but a group of diseases. Usually, Cushing syndrome results from certain medications that lead to high levels of cortisol in the body.
What is the role of cortisol in the body?
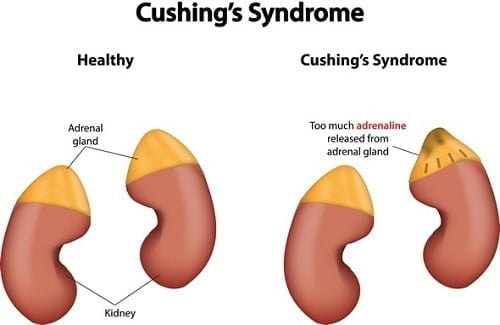
The hormone cortisol is produced by the outer layer of adrenal glands, known as the cortex. Cortisol is a steroid hormone that helps in the breakdown of fats and protein. It also helps the body to respond to physical and emotional stress, regulation of blood pressure, and management of cardiovascular function. The adrenal glands are located on the top of each kidney.
Cortisol is also known as the stress hormone. It secreted by the adrenal glands, triangle-shaped organs located at the top of the kidneys. It plays an important role in the following types of processes going on in the body:
-
Utilization of carbohydrates, fats, and proteins.
-
Reduction in the inflammation
-
Regulation of blood pressure
-
Increase in the blood sugar
-
Management of sleep cycle and biological clock of the body.
-
Provides energy to handle stress
Possible causes of Cushing’s syndrome
Cushing disease – Cushing disease is caused by the pituitary gland that produces an excess amount of ACTH hormone, which provides signals to the adrenal gland to produce cortisol. This is the most common cause for endogenous cortisol production by the adrenal glands.
Presence of tumor – Any tumor in the adrenal gland or adrenal hyperplasia can lead to overproduction of cortisol. In addition to this, any tumor in any other part of the body such as the pancreas, lungs or thyroid can also stimulate the production of ACTH.
Prolonged glucocorticoid therapy – Cushing syndrome may also occur as a result of taking glucocorticoid hormones. These hormones are chemically similar to the natural cortisol. The glucocorticoid hormones include medications such as prednisone that are usually prescribed for asthma, rheumatoid arthritis, lupus or other inflammatory diseases. Such hormones are also taken after an organ transplant to suppress the immune rejection of the transplanted organ.
Who is more prone to have Cushing syndrome?
As per the statistics, the condition is frequently observed in adults of age 20-50 years. Moreover, it is 3 times more common in women than in men. People who are obese and have type 2 diabetes are also more prone to have Cushing syndrome. In rare cases, a person may also have an inherited gene mutation like Multiple Endocrine Neoplasia Type 1 (MEN-1). MEN-1 elevates the risk of developing tumor throughout the endocrine system, which includes pituitary and adrenal tumors.
10 most common signs and symptoms indicating Cushing syndrome
Following are the warning signs indicating that you must consult an endocrinologist.
-
Round or moon-shaped face
-
Extra fat accumulation in the neck and shoulder area
-
Visual changes like glaucoma or cataract
-
Increased risk of infection
-
Obesity in the central body with thinner arms and legs
-
Increased thirst and excessive urination
-
Pink or purple colored streaks like stretch marks on the abdomen, thighs, and buttocks
-
Thin fragile skin, which is gets bruised easily
-
Hirsutism and irregular menstrual cycles in women
-
Erectile dysfunction and reduced libido in men
Some other symptoms associated with Cushing syndrome are:
-
Muscle weakness
-
Decreased endurance
-
Osteoporosis
-
Raised blood pressure
-
Elevated blood sugar levels
-
Headache
-
Back pain
-
Slow growth in children with Cushing syndrome
-
Mental ill health
-
Acne
-
Gradual healing of cuts, insect bites and infections.
-
Excessive fatigue
-
Depression, anxiety, and irritability
How is Cushing Syndrome Diagnosed?
If you notice one or more of the aforementioned signs and symptoms, you must consult an endocrinologist. The doctor will take a detailed case history in which he/she will ask the patient about any other medical conditions. One must tell the doctor all the details regarding any past medical illness or any family history. This is followed by a physical examination in which the physician will look for the moon-shaped face, fatty tissue around the neck or shoulders, and skin with bruises or stretch marks. Furthermore, some lab tests are also conducted such as,
Urine and blood tests – These tests are carried out to measure hormone levels in the urine and in the blood. The urine is collected within 24 hours before the test.
Saliva test – Normally, cortisol levels drop considerably by the evening. Hence, samples of saliva are tested at late at night. If the cortisol levels are too high, it indicates a positive result for Cushing syndrome.
Dexamethasone suppression test – The patient is asked to take a low dose of steroid pill at 11 pm and the blood sample is taken in the morning to measure the amount of cortisol produced by the body. This test also distinguishes Cushing syndrome from Pseudo-Cushing syndrome.
Radio-imaging tests – Tests such as a CT scan or MRI scan help by providing images of pituitary and adrenal glands to detect abnormalities like tumors.
Petrosal sinus sampling – This test is done in cases of endogenous Cushing syndrome to know whether the source is a pituitary gland or adrenal gland. Blood samples are taken from the petrosal sinuses that drain the pituitary gland.
A narrow tube is inserted through the upper thigh after sedation. The levels of ACTH are measured from the sinus. If the levels are high in the sinus sample, the origin lies in the pituitary gland and if the ACTH levels are similar between sinus and forearm, origin lies outside the pituitary gland.
Treatment
The goal of the treatment is to reduce the elevated levels of cortisol. The best endocrinologists in India have come up with the following treatment choices to treat the patient with Cushing syndrome.
Decreased use of corticosteroid – Cases in which the cause is long-term use of corticosteroids medication, the doctor may ask you to reduce the dosage and sometimes replace it with non-corticosteroid medications. Corticosteroid medications are tapered down slowly instead of discontinuing abruptly.
Surgery – Surgery is the choice of treatment when the cause is a tumor. A tumor present in the pituitary gland is removed by a neurosurgeon. The procedure is performed through the nose. If the tumor is present in the adrenal gland, lungs or pancreas, standard techniques may be followed with minimal invasion using small incisions. The patients are given cortisol replacement medications to provide the correct amount of cortisol. The entire process can take up to a year or longer.
Radiation therapy – This is also used in cases of tumors in addition to surgical removal. The radiation is given in small doses over a period of 6 weeks. This is known as stereotactic radiosurgery.
Medications – Drugs like ketoconazole, mitotane, and metyrapone are used to control the production of cortisol by the adrenal gland. Also, mifepristone is used for those who have a history of type 2 diabetes or glucose intolerance.